Immune Responses to Tumors
Immune Responses to Tumors
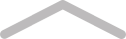
Adaptive immune responses, mainly mediated by T cells, have been shown to control the development and progression of malignant tumors. Both innate and adaptive immune responses can be detected in patients and experimental animals, and various immune mechanisms can kill tumor cells in vitro. The challenge for tumor immunologists is to determine which of these mechanisms may contribute significantly to protection against tumors and to enhance these effector mechanisms in ways that are tumor specific. (Figure 1)
1. T Lymphocytes
The principal mechanism of adaptive immune protection against tumors is killing of tumor cells by CD8+ CTLs. CTLs may perform a surveillance function by recognizing and killing potentially malignant cells that express peptides that are derived from tumor antigens and are presented in association with class I MHC molecules. CD8+ T cell responses specific for tumor antigens may require cross-presentation of the tumor antigens by dendritic cells. Most tumor cells are not derived from APCs and therefore do not express the costimulators needed to initiate T cell responses or the class II MHC molecules needed to stimulate helper T cells that promote the differentiation of CD8+ T cells. A likely explanation of how T cell responses to tumors are initiated is that tumor cells or their antigens are ingested by host APCs, particularly dendritic cells, and tumor antigens are processed inside the APCs. Peptides derived from these antigens are then displayed bound to class I MHC molecules for recognition by CD8+ T cells. The APCs express costimulators that provide the signals needed for differentiation of CD8+ T cells into anti-tumor CTLs.
The importance of CD4+ helper T cells in tumor immunity is less clear. CD4+ cells may play a role in anti-tumor immune responses by providing cytokines for differentiation of naive CD8+ T cells into effector and memory CTLs. In addition, helper T cells specific for tumor antigens may secrete cytokines, such as TNF and IFN-γ, that can increase tumor cell class I MHC expression and sensitivity to lysis by CTLs.
2. Antibody
Tumor-bearing hosts may produce antibodies against various tumor antigens. For example, patients with EBV associated lymphomas have serum antibodies against EBV-encoded antigens expressed on the surface of the lymphoma cells. Antibodies may kill tumor cells by activating complement or by antibody-dependent cell-mediated cytotoxicity, in which Fc receptor–bearing macrophages or NK cells mediate the killing. However, the ability of antibodies to eliminate tumor cells has been demonstrated largely in vitro, and there is little evidence for effective humoral immune responses against tumors.
3. Natural Killer Cell
NK cells kill many types of tumor cells, especially cells that have reduced class I MHC expression and express ligands for NK cell–activating receptors. The importance of NK cells in tumor immunity in vivo is unclear. In some studies, T cell–deficient mice do not have a high incidence of spontaneous tumors, and this is attributed to the presence of normal numbers of NK cells that serve an immune surveillance function.
4. Macrophages
Macrophages are capable of both inhibiting and promoting the growth and spread of cancers, depending on their activation state. Classically activated M1 macrophages, discussed in Chapter 10, can kill many tumor cells. How macrophages are activated by tumors is not known. Possible mechanisms include recognition of damage-associated molecular patterns from dying tumor cells by macrophage TLRs and other innate immune receptors, and activation of macrophages by IFN-γ produced by tumor-specific T cells. M1 macrophages can kill tumor cells by mechanisms that they also use to kill infectious organisms.
There is evidence that some macrophages in tumors contribute to tumor progression and have an M2 phenotype. These cells secrete vascular endothelial growth factor (VEGF), transforming growth factor-β (TGF-β), and other soluble factors that promote tumor angiogenesis.
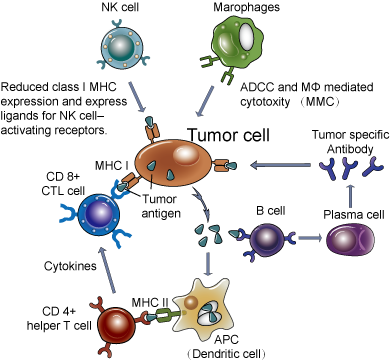
Figure 1. Immune response to tumor.
Evasion of Immune Responses by Tumors
Many cancers develop mechanisms that allow them to evade anti-tumor immune responses. These mechanisms can broadly be divided into those that are intrinsic to the tumor cells and those that are mediated by other cells (Fig. 2). A major focus of tumor immunology is to understand the immune evasion mechanisms of tumors, with the hope that interventions to prevent immune evasion will increase the immunogenicity of tumors and maximize the responses of the host.
1. Escaping Immune Recognition by Loss of Antigen Expression
Immune responses to tumor cells impart selective pressures that result in the survival and outgrowth of variant tumor cells with reduced immunogenicity, a process that has been called tumor immunoediting. Tumors developing in the setting of a normal immune system become less immunogenic over time, which is consistent with the selection of less immunogenic variant cells. Given the high mitotic rate of tumor cells and their genetic instability, mutations or deletions in genes encoding tumor antigens are common. If these antigens are not required for growth of the tumors or maintenance of the transformed phenotype, the antigen-negative tumor cells will have a growth advantage in the face of the host immune system. Thus, tumor immunoediting is thought to underlie the emergence of tumors that escape immune surveillance.
In addition to loss of tumor-specific antigens, class I MHC expression may be down-regulated on tumor cells so that they cannot be recognized by CTLs. Various tumors show decreased synthesis of class I MHC molecules, β2-microglobulin, or components of the antigen processing machinery, including the transporter associated with antigen processing and some subunits of the proteasome. These mechanisms are presumably adaptations of the tumors that arise in response to the selection pressures of host immunity, and they may allow tumor cells to evade T cell–mediated immune responses.
2. Active Inhibition of Immune Responses
Tumors may engage inhibitory mechanisms that suppress immune responses. There is strong experimental and clinical evidence that T cell responses to some tumors are inhibited by the involvement of CTLA-4 or PD-1, two of the best-defined inhibitory pathways in T cells. Secreted products of tumor cells may suppress antitumor immune responses. Regulatory T cells may suppress T cell responses to tumors. Tumor-associated macrophages may promote tumor growth and invasiveness by altering the tissue microenvironment and by suppressing T cell responses. Myeloid-derived suppressor cells (MDSCs) are immature myeloid precursors that are recruited from the bone marrow and accumulate in lymphoid tissues, blood, or tumors of tumor-bearing animals and cancer patients and suppress anti-tumor innate and T cell responses.
Figure 2. Evasion mechanisms of immune responses by tumors.
Immunotherapy for Tumors
The potential for treatment of cancer patients by immunologic approaches has held great promise for oncologists and immunologists for many years. The main reason for interest in an immunologic approach is that most current therapies for cancer rely on drugs that kill dividing cells or block cell division, and these treatments have harmful effects on normal proliferating cells. As a result, the treatment of cancers causes significant morbidity and mortality. Immune responses to tumors may be specific for tumor antigens and will not injure most of the normal cells. Therefore, immunotherapy has the potential of being the most tumor-specific treatment that can be devised. Advances in our understanding of the immune system and in defining antigens on tumor cells have encouraged many new strategies. Immunotherapy for tumors aims to augment the weak host immune response to the tumors (active immunity) or to administer tumor-specific antibodies or T cells, a form of passive immunity.
Browse All Products Related to Cancer Biomarkers
Browse All Products Related to Tumor Marker ELISA Kit
Browse All Products Related to Tumor Marker RDT
Article source: https://www.creative-diagnostics.com/Tumor-Immunity.htm
References:
1.Murphy K M. Janeway’s immunobiology[M]. Garland Science, 2011.
2.Abbas A K, Lichtman A H H, Pillai S. Cellular and Molecular Immunology: with STUDENT CONSULT Online Access[M]. Elsevier Health Sciences, 2014.